Melasma 101: Causes, Triggers, and Why It’s So Hard to Treat
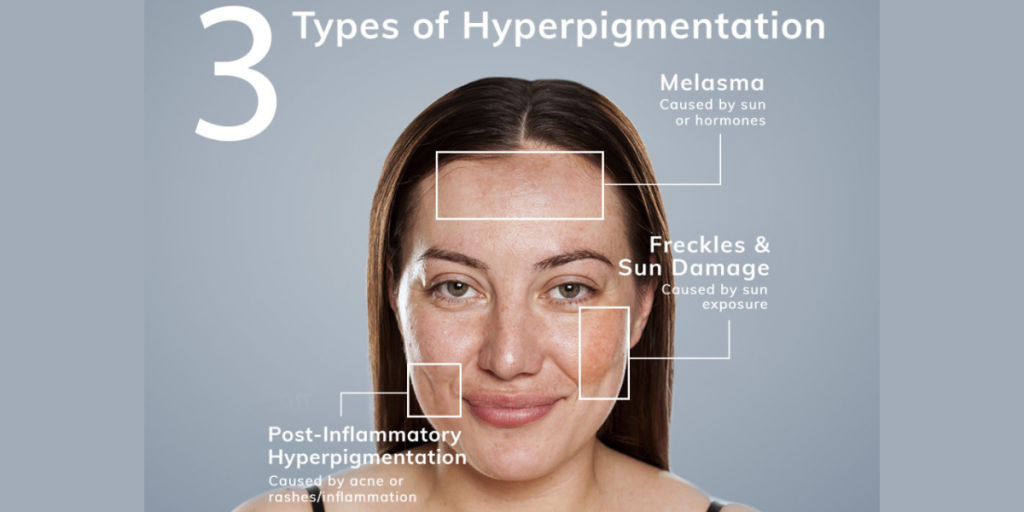
Melasma (best treatment for melasma on face) is one of the most stubborn forms of facial hyperpigmentation. Those symmetrical brown or gray‑brown patches—often on the cheeks, forehead, nose, and upper lip—can fade, flare, and come back without warning. Understanding what drives melasma is the first step to managing it well.
What is melasma?
Melasma is a chronic pigmentation disorder where melanocytes (the pigment-producing cells) become overactive. It’s more common in women, in skin of color (Fitzpatrick III–VI), and in people with a family history. Under the microscope, melasma involves more than “extra pigment”—there are inflammatory and vascular changes, weakened skin support structures, and sometimes pigment that has dropped into the dermis. That complexity explains why it’s slow to treat and easy to relapse.
Classic patterns:
– Centrofacial: forehead, cheeks, nose, upper lip, chin
– Malar: cheeks and nose
– Mandibular: jawline (less common)
Causes and risk factors
There isn’t a single cause; melasma happens when a predisposition meets the right triggers.
– Genetics: Family history raises risk.
– Hormones: Pregnancy, oral contraceptives, and hormone therapy can stimulate melanocytes via estrogen/progesterone pathways.
– UV and visible light: UVA/UVB and high‑energy visible (blue) light both increase pigment production.
– Heat and inflammation: Heat (sun, saunas, hot yoga, even steamy kitchens) and low‑grade inflammation can worsen melasma.
– Medications and products: Some drugs and fragrances can increase photosensitivity and pigment.
– Thyroid and vascular factors: Studies suggest associations with thyroid autoimmunity and increased skin vascularity in melasma patches.
Common triggers you can actually control
– Sunlight year‑round, including through windows
– Visible light from screens/indoor lighting (less potent than sun, but still contributory)
– Heat exposure and friction (e.g., aggressive scrubbing, hot wax)
– Irritating skincare routines that damage the barrier and provoke inflammation
Why is melasma so hard to treat
– Mixed depth pigment: Epidermal pigment lightens faster; dermal/mixed pigment is slower and more relapse‑prone.
– Constant triggers: You can’t fully avoid sunlight or heat, so maintenance matters.
– Sensitive skin barrier: Irritation itself drives pigment, limiting how aggressive you can be.
– Risk of rebound: Some procedures (and even strong topicals) can clear quickly but trigger relapse or post‑inflammatory hyperpigmentation (PIH), especially in deeper skin tones.
– It’s chronic: Melasma behaves more like a condition to manage than a “one‑and‑done” problem.

An evidence‑based approach to managing melasma
Think of pillars as protecting, lighting, calming, and maintaining.
1) Daily protection (non‑negotiable)
– Broad‑spectrum SPF 50+ with protection against UVA, UVB, and visible light. Select a tinted sunscreen containing iron oxides for effective coverage of visible light.
– Reapply every 2–3 hours when outdoors; use hats and shade.
– Manage heat: favor cooler workouts, avoid steam/saunas when flaring.
2) Proven topical treatments
– Hydroquinone 2–4%: Still a gold standard for short cycles (e.g., 8–12 weeks), then break to limit irritation/ochronosis risk.
– Triple combination cream (hydroquinone + tretinoin + mild steroid): Powerful for moderate–severe cases; best under dermatology supervision and used time‑limited.
– Azelaic acid 15–20%: Brightens with anti‑inflammatory benefits; safe for long‑term use and during pregnancy.
– Tranexamic acid (topical 2–5%): Helps reduce vascular/inflammatory drivers; oral TXA can be considered under physician care.
– Cysteamine 5%: A useful option for stubborn cases; often applied nightly in short contact.
– Support actives: Retinoids (tretinoin/adapalene/retinal), vitamin C, niacinamide, kojic acid, arbutin, licorice extract. These help pigmentation and barrier health.
Barrier‑smart routine:
– Gentle, non‑foaming cleanser
– Antioxidant/niacinamide in the morning under sunscreen
– Moisturizer with ceramides to minimize irritation from actives
– Introduce one new active at a time; back off if stinging or redness persists
3) In‑office procedures (use judiciously)
– Superficial chemical peels (glycolic, mandelic, lactic, Jessner’s): Can speed fading when skin is well‑prepped; avoid medium–deep peels for melasma (best treatment for melasma on face).
– Low‑fluence 1064 nm Q‑switched Nd:YAG (“laser toning”) and non‑ablative fractional lasers (e.g., 1927 nm thulium): May help select cases but carry rebound risk. Best for patients who have maximized topical care and strict sun protection.
– Microneedling with topical tranexamic acid: An option for some, with less heat than lasers.
4) Maintenance (the long game)
– Keep photoprotection daily, even after clearing.
– Rotate gentle brighteners (azelaic acid, niacinamide, vitamin C) between more intensive cycles.
– Expect fluctuations with seasons/hormonal shifts; tweak your routine accordingly.
When to avoid or modify:
– Pregnancy/postpartum: Skip hydroquinone/retinoids; choose azelaic acid, vitamin C, niacinamide, strict sun protection.
– Skin of color: Favor gentle, anti‑inflammatory regimens and superficial peels to reduce PIH risk.
– Clotting risk: Oral tranexamic acid is prescription‑only and not suitable for everyone.
How long until you see results?
With consistent care, many people notice improvement within 8–12 weeks. Deeper or long‑standing melasma may need several months and a maintenance plan to hold results.
When to see a dermatologist (best treatment for melasma on face)
– Rapidly changing or atypical spots
– Melasma unresponsive to 3 months of diligent care
– Considering oral tranexamic acid, compounded triple therapy, or procedures
– You’re unsure if your dark patches are melasma, sun spots, or PIH
Note: This information is educational and not a substitute for personalized medical advice.
Melasma dark spots on face
Melasma often appears as symmetrical dark patches on the cheeks, forehead, bridge of the nose, and upper lip, giving a “mask‑like” look. Unlike simple sun spots, melasma tends to darken with heat and even brief sun exposure, then fade slowly over weeks. It’s driven by overactive pigment cells plus inflammation and increased skin vascularity, which is why gentle routines and daily tinted SPF 50+ are essential. If your dark spots are blotchy, occur in mirror‑image patterns, and worsen in summer or with hormones, melasma is likely—though a dermatologist can confirm and tailor treatment.
Chemical peel for melasma
Superficial chemical peels—such as glycolic (20–35%), mandelic (20–40%), lactic, or Jessner’s—can safely speed up melasma clearance by accelerating cell turnover and enhancing penetration of brightening creams. The best outcomes come from a series of gentle peels spaced 3–4 weeks apart, combined with a solid home routine (tinted SPF, azelaic acid or hydroquinone cycles, retinoids if appropriate). Avoid deeper peels and aggressive strengths that raise the risk of post‑inflammatory hyperpigmentation, especially in darker skin tones. Pre‑ and post‑peel sun protection and barrier care are non‑negotiable.
How Many Sessions Do You Need for Melasma
Treatment is individualized, but most in‑office options work best in a series. Superficial chemical peels typically require 3–6 sessions (every 3–4 weeks). Low‑fluence 1064 nm laser toning often needs 5–10 sessions (1–2 weeks apart) with careful maintenance to prevent rebound. Microneedling protocols usually involve 3–4 monthly sessions. Regardless of the procedure, results depend heavily on strict daily tinted SPF, heat management, and a consistent topical routine.
What Does It Cost?
(best treatment for melasma on face) Costs can vary depending on the clinic, city, and type of treatment. As a general guide in India, over-the-counter skin brightening creams and sunscreens usually range from ₹500–₹3,000 each. Prescription or dermatologist-compounded creams (like triple-combination formulas) may cost around ₹1,500–₹6,000 per month. If your doctor recommends oral tranexamic acid, it’s typically ₹500–₹2,000 per month.
For in-clinic procedures, prices differ based on the technology and number of sessions. Superficial chemical peels generally cost ₹3,000–₹10,000 per session, microneedling around ₹7,000–₹20,000, laser toning about ₹10,000–₹30,000, and fractional thulium or resurfacing lasers can range from ₹20,000–₹80,000 per session.
Many clinics offer discounted packages or combination treatments, which can lower the overall cost. Remember — consistent maintenance and daily sun protection are key investments to keep your skin healthy and preserve your results.
Committed to Excellence in Healthcare
At Pyramid Healthcare, we believe that good health is the foundation of a happy life. Our mission is simple — to care for every person with compassion, honesty, and expertise. From routine check-ups to advanced medical treatments, our team of experienced doctors and caregivers works together to ensure that every patient feels supported and heard. We combine modern medical technology with a personal touch, creating a healing environment where comfort and trust come first. At Pyramid Healthcare, you’re not just another case — you’re family, and your well-being is at the heart of everything we do.
 Skip to content
Skip to content